For most of us, the story is familiar. We go for a routine check-up, get a few standard blood tests, and leave with a conclusion that sounds reassuring, or a prescription that promises to “fix the numbers.” Cholesterol slightly high? Statins. Thyroid a bit off? Hormones. Blood sugar creeping up? Watch it… or medicate it.
What rarely happens is a deeper conversation about why those numbers are changing in the first place. This is where biomarker testing changes everything.
Biomarkers don’t just tell us what is happening in the body. They help explain why it’s happening, which biological system is under stress, and how early the imbalance began. That difference, between treating outcomes and understanding causes, is the foundation of modern longevity and preventive medicine.
From reactive care to root-cause insight
Conventional healthcare is largely reactive. It waits for symptoms to appear or for values to cross a diagnostic threshold. By the time that happens, dysfunction has often been developing silently for years.
Biomarker-driven care flips this logic. Instead of asking whether a value is “high enough to treat,” it asks whether the body is still functioning optimally. It looks at inflammation before disease, insulin resistance before diabetes, vascular stress before cardiovascular events, and hormonal shifts before burnout or metabolic decline.
This is why advanced biomarker analysis is now considered the gold standard for longevity. Not because it replaces doctors or medications, but because it gives context, timing, and causality, three things traditional check-ups often miss.
Why cholesterol alone is not the full story
Take cholesterol as an example. In a typical visit, LDL cholesterol becomes the main character. But LDL alone doesn’t tell us whether the risk is driven by inflammation, insulin resistance, oxidative stress, liver dysfunction, or genetic lipid transport issues.
Advanced cardiovascular biomarkers look at cholesterol particles, ratios, apolipoproteins, triglyceride dynamics, and inflammatory interactions. This matters because two people can have the same LDL value and very different cardiovascular risk.
Lowering LDL without understanding these drivers can improve a lab report while leaving the underlying problem untouched. Numbers look better. Biology doesn’t.
What comprehensive biomarker testing actually reveals
Platforms like Superpower reflect a growing shift toward systems-based health analysis. Instead of fragmented tests, biomarkers are interpreted together, cardiovascular, metabolic, hormonal, inflammatory, thyroid, liver, kidney, immune, nutrient, and even aging-related markers.
What makes this approach powerful is not the number of tests, but how they are read in relation to each other. Patterns emerge. Connections become visible. Early dysfunction shows up before it becomes a diagnosis.
A slightly elevated inflammatory marker alongside subtle insulin resistance and liver stress tells a very different story than a single abnormal value viewed in isolation. This kind of interpretation moves health care from reaction to prevention.
Why most people don’t get access to this level of insight
The reason advanced biomarker testing isn’t part of routine care is not lack of science, it’s system design. Preventive interpretation takes time. It requires depth, longitudinal thinking, and personalized context. These are not things most healthcare systems are built to prioritize or reimburse.
Doctors are trained to diagnose and treat disease, not always to map early dysfunction. Appointments are short. Guidelines are rigid. Prevention often falls outside the system, even though it’s where the biggest impact lies.
That gap is where biomarker-based longevity medicine has emerged.
The shift that gives people hope again
What’s changing is not just technology, but mindset. People are no longer satisfied with being told to “wait and see” or to medicate symptoms without understanding the cause. They want to know what’s happening inside their bodies, how lifestyle and environment interact with biology, and how to intervene before health declines.
This shift is not anti-medicine. It’s pro-understanding.
Biological age is not destiny. It’s feedback.
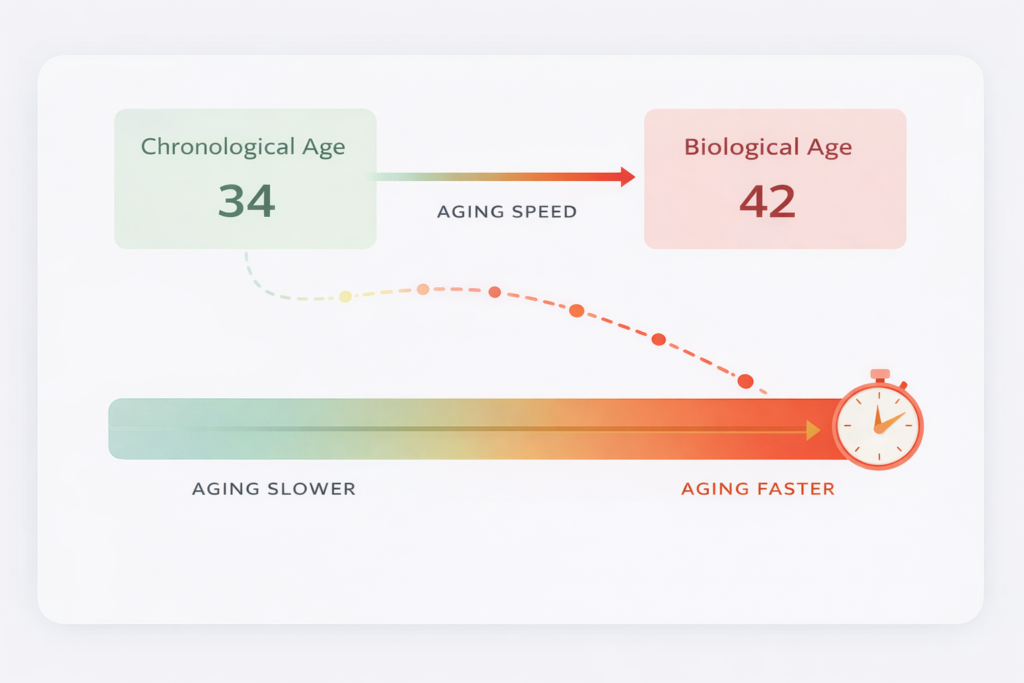
Biological age is not guessed. It is calculated using algorithms developed from large population datasets that track how specific biomarkers change over time. One of the most influential approaches comes from research led by Professor Morgan Levine at Yale School of Medicine, who developed biological age models based on patterns across clinical biomarkers such as inflammation markers, glucose regulation, kidney function, albumin levels, and blood cell indices. Instead of looking at one value in isolation, the algorithm analyzes how multiple systems are performing together and compares that pattern to population-level aging data.
In simple terms, your biological age reflects how your internal systems are functioning relative to your chronological peers. If inflammation, metabolic markers, and organ function resemble those typically seen in younger individuals, your biological age trends lower. If multiple systems show accelerated wear, it trends higher.
This is powerful because it shifts the focus from “How old am I?” to “How fast am I aging, and can I influence that rate?”
What Kungul believes about prevention
Kungul was built for the moment when someone looks at a label and realizes: “I don’t actually know what I’m choosing.” Health works the same way. A short lab panel can look normal while the biology underneath is already shifting, slowly, silently, and predictably.
We don’t believe in fear-based health. We believe in clarity.
Biomarkers are clarity. They show patterns before they become diagnosed. They help you stop guessing and start acting early, together with your doctor, not instead of one. The same way Kungul teaches you to read an ingredient list beyond marketing, biomarkers teach you to read your body beyond “normal ranges.” Both are about the same thing: not waiting until the damage is loud. Before jumping into the latest longevity trend, it’s worth reading our take on biohackers, influencers, and the truth about supplements to understand where science ends and marketing begins.
What I wish more people knew
Lowering a number is not the same as getting healthier. Sometimes medication is necessary. Sometimes it’s lifesaving. But if you never ask why a value rose in the first place, you end up chasing fixes while the cause keeps running quietly in the background.
Biomarkers bring that cause to the surface.
They don’t promise perfection. They offer understanding. And once you understand what’s driving the imbalance, you can change the trajectory, not just the result.Health doesn’t fail suddenly. It whispers first.
Biomarkers help you hear it in time.